FAQs
Browse the sections below for detailed answers organized by topic to address common questions regarding assessments, fees, accommodations and more. If you have additional questions or require further assistance, please don't hesitate to contact ABIM.
Accreditation Council for Continuing Medical Education (ACCME) Collaboration
Visit CME Passport to search the list of continuing medical education (CME) activities that earn ABIM Maintenance of Certification (MOC) points.
You can filter the list of activities by fields such as specialty, CME provider (e.g., professional membership organization and/or affiliation), activity type, credit type, fee and location.
You can also contact the CME provider to inquire about ABIM MOC eligibility for a specific activity. Check for the CME Accredited/ABIM MOC badge (above) on activity materials, brochures and announcements.
The CME provider is responsible for collecting and submitting your activity completion information, so it is best to contact the CME provider to inquire about how to claim MOC points for a specific activity. You do not need to contact ABIM to claim MOC points.
First, check to be sure that your fees are paid. ABIM does not process MOC points until your fees are paid.
If your fees are up to date, it is best to contact the CME provider to inquire about their timeframe for submission of completion information for a specific activity.
The timeframe for submission of completion information varies by activity and can depend on how the CME provider reports completion information. For example:
- Some CME providers use web services to transmit completion information from their software applications or learning management systems, often resulting in MOC points being awarded within 24 hours of activity completion.
- Other CME providers submit periodic batch reports, which may result in a longer lag time from activity completion to the awarding of MOC points.
- Some CME providers require you to initiate or authorize the submission of MOC points in some way prior to sending your completion information to ABIM.
CME providers are encouraged to submit completion information as soon as possible after the CME activity is completed so that MOC points can be awarded. MOC points earned for CME activities completed by December 31 will count towards any MOC requirements that are due by the end of the year. If you experience a status change as a direct result of insufficient MOC points, your status will be adjusted once the required number of points have been earned.
You will receive an email with the subject line “You Earned ABIM MOC Points For Activity Completion” to notify you that MOC points have recently been granted.
You can also check to see if the CME provider has submitted your completion information by signing in to your Physician Portal and going to "My Activities."
If the CME provider has submitted your MOC points and you did not receive an email notification and do not see them in the My Activities section of your Physician Portal, then check to see whether your fees are paid. ABIM does not process MOC points until your fees have been paid.
No, ABIM cannot award MOC points based on submission of CME certificates. The CME provider will collect and submit your completion information so that ABIM may award your MOC points.
The CME provider determines the deadline for claiming MOC points for an activity. It is best to contact the CME provider to inquire about the deadline for a specific CME activity.
ABIM does not have any restrictions that preclude CME providers from reporting MOC points for activities completed in prior years. Since the CME provider determines the deadline for claiming MOC points for an activity, and it may take time for the CME provider to adjust their systems and processes to accommodate the reporting of activities completed in prior years, it is best to contact the CME provider to inquire about claiming MOC points for a specific activity.
ABIM MOC registration is open to all CME providers accredited within the ACCME system, however, it is voluntary. The CME providers determine which of their activities meet ABIM's requirements in support of physician engagement in lifelong learning and quality improvement.
It may take CME providers time to implement ABIM's requirements in their CME programs and build the infrastructure to capture completion information for the purpose of reporting MOC credit to ABIM.
If your organization is not aware of the ABIM MOC opportunity, you might consider sharing the CME for MOC Program Guide and directing them to ACCME for additional information about this opportunity.
Once an activity has ended, it is no longer searchable in CME Passport. Contact the CME provider to inquire about ABIM MOC eligibility for a specific activity.
Many CME activities allow you to earn MOC points, including:
- Live and online courses
- Going to society meetings in a live or virtual setting
- Grand Rounds and Tumor Boards (e.g., regularly scheduled series)
- Quality improvement/performance improvement (QI/PI) activities
- Reading journal articles
- Internet search tools that support clinical decisions at the point of care
- Item-writing
- Committee learning
- Manuscript review
- Learning from teaching
Many CME activities allow you to earn MOC points over time. Examples include:
- Sections or modules within an enduring material
- Grand Rounds
- Journal-based CME
- Internet searching and learning tools
MOC points earned for a CME activity may be aggregated (rolled up) on a monthly or annual basis in the My Activities section of your Physician Portal. The report will display the total points earned for the activity during the month or year as well as the most recent date that points were earned.
Yes. CME providers can request removal of MOC points that were previously awarded in error, but only within the current calendar year (points cannot be removed from prior calendar years). You will receive an email notification with the subject line “MOC Points Removed” advising you to contact the CME provider if you have questions about why the points were removed. You may also see negative points or zero points displayed in the My Activities section of your Physician Portal when MOC points have been removed.
Accommodations
In fairness to all candidates and to help ensure the integrity of the certification process, ABIM examinations are only available on computer. ABIM considers the full range of available accommodations to assist candidates with disabilities. Providing a paper-assisted exam is very difficult and usually not considered a reasonable accommodation.
No, ABIM does not charge to grant accommodations. However, the supporting medical documentation required for your request is obtained at your expense.
Send an email to the ABIM Special Exams Coordinator at accommodations@abim.org to discuss your options. We will work to find the best solution for your testing needs.
Food and drinks are not permitted in Pearson VUE testing rooms. If there is a medical necessity to have these items, then an accommodation request must be submitted by completing the comfort aid form (pdf).
Pearson VUE does not require candidates to seek prior approval from ABIM in order to bring certain comfort aids into the testing room. You can view a list of comfort aids that Pearson VUE has allowed in the past. If there is a medical necessity to have an item, then an accommodation request must be submitted by completing the comfort aid form (pdf).
Candidates seeking accommodations for multiple impairments that fall into two or more categories should submit one request but supply supporting documentation for each disability.
If you are uncertain into which category your impairment or condition falls, please contact the ABIM Special Exams Coordinator at accommodations@abim.org for guidance.
Yes. ABIM will offer accommodations for the Longitudinal Knowledge Assessment (LKA®) in compliance with Title III of the Americans with Disabilities Act (ADA) for individuals with documented disabilities who demonstrate a need for accommodation. Given the format of the LKA, some common testing accommodations may not be available.
Physicians requesting special testing accommodations under the ADA should submit a completed request by the deadline.
Learn more about ABIM’s evaluation of accommodations requests.
Due to its format, certain accommodations may not be available for the LKA. ABIM will ensure that physicians with a disability have access to auxiliary aids and services in accordance with Title III, but devices and services of a personal nature must be provided by the physician. For example, the availability of a computer with broadband access is necessary for the LKA, but these would be considered personal devices or services that the physician is responsible for arranging.
If approved for additional testing time, the time will be added to the standard five minutes that physicians have to answer each question as well as the 30-minute time bank physicians may access each year if more time is needed on a particular question.
Accommodations previously approved by ABIM may not automatically apply to the LKA due to its format. Upon enrollment in the LKA, ABIM’s accommodations team will review your approval history and provide a new determination for this assessment only.
The LKA is designed to work with most text-to-speech and screen magnification programs. You may also adjust the font size with your keyboard.
For additional information, please contact accommodations@abim.org.
ACC/ABIM Collaborative Maintenance Pathway (CMP)
The CMP Performance Assessment (PA) will cover approximately 20% of the field annually.
No, if you pass the CMP Performance Assessment each year, you won’t need to take another ABIM assessment option to maintain your certification.
Yes, you have the option to switch back to ABIM’s assessment. Please contact the American College of Cardiology (ACC) to un-enroll from the CMP so you can then register for an ABIM assessment (subject to availability).
Yes. You have two hours to complete 60 questions.
Most participants will receive immediate feedback about whether they pass. The scores of some participants will require additional analysis and they will not learn immediately whether they passed. They will learn their status via the Score Report.
Two weeks after the testing window closes, ACC will release score reports with the following information:
- Your scaled score
- The passing scaled score
- Recommended content for further study based on areas of weakness.
ACC will email all participants when the score report is available within the CMP Hub.
If you do not pass a CMP PA in the year that your assessment requirement is due, you will not lose your certification. Instead, you will need to take the ABIM traditional, 10-year MOC exam and achieve a passing score. After passing the MOC exam, you can return to the CMP.
You can begin the CMP at any time but you are not required to do anything before the year your assessment is due. As long as you pass in the year your assessment is due, you will be reported as meeting your assessment requirement.
No. Currently, the only pathways to reinstate a lapsed certificate are to:
- Take and pass the traditional, 10-year MOC exam; or,
- Participate in the LKA.
FasTrack®
Submitting outstanding evaluations after published deadlines puts trainee certification eligibility at risk. Residents and fellows with incomplete training will not be eligible for board certification.
The Internal Medicine Certification Examination occurs shortly after ABIM receives and loads evaluation data sent by the Accreditation Council for Graduate Medical Education (ACGME). In recognition of this short period for turnaround, ABIM will grant admission/reject admission to the Internal Medicine Certification Examination based on information transferred to ABIM from ACGME's Accreditation Data System (ADS) in July, and candidate certification will be granted pending submission of the evaluation by the program.
Candidates will be informed of examination results pending submission of the evaluation by the program.
The internal medicine deadline falls on June 30 because ABIM will not have evaluation information on trainees upon which to base eligibility decisions until the non-ACGME-accredited program submits them to ABIM.
Yes, you must continue to submit information to ACGME through the Accreditation Data System (ADS).
Up to four users can be associated with FasTrack per training program, and users are identified in the system by their unique email address. A role must be assigned to each user, with the program director and program coordinator retaining the ability to submit evaluations and add/remove users. The “other” role may be assigned to staff or faculty, and is essentially a data entry role that has read/write/edit/save access to FasTrack. Please do not share account information. Only designated FasTrack users should be logging into FasTrack and working with trainee information.
FasTrack user accounts are managed via the Accounts/Settings link in the upper right corner of the FasTrack screen. When entering a new FasTrack user, remember to select the “Save” button at the top of the Accounts/Settings page before leaving the screen.
FasTrack's default start and end dates for the academic year are July 1 of the previous year and June 30 of the current year. Programs may change the start and end dates for all of their trainees by using the Accounts/Settings link in the upper right corner of the FasTrack screen. When changing these dates, remember to select the “Save” button at the top of the Accounts/Settings page before leaving the screen.
The start and end dates entered into Accounts/Settings will be reflected on all evaluations loaded into FasTrack after those changes were made and saved in Accounts/Settings. FasTrack users can still make changes to individual trainee records, for instance, if a trainee is off the normal academic cycle.
MOC Fee
You can pay the annual MOC fee during the calendar year in which it is due, before it is due or after it is due. The annual fee for the first certificate you maintain is $220, including access to the LKA. For each additional certificate you maintain, the annual fee is $120 per year including access to the LKA. An additional $40 will be added to the certificate fee if it is paid after the year in which it was due.
If you choose to pay in advance, you will receive a 5% discount for each year paid (up to nine years) before the year in which it is due.
For those choosing to take the traditional, 10-year MOC exam, there is a $700 test center fee due upon registration.
Your certification status will never change due to non-payment. However, you will not be able to access some of the services ABIM provides:
- The ability to answer LKA questions (you will continue to have access to your LKA dashboard but cannot open the questions).
- Registering for an MOC assessment.
- Processing MOC points for CME activities.
- Enrolling in the MOC reciprocity program.
For those with an exam credit from a Knowledge Check-In or traditional, 10-year MOC exam, you will not be charged an additional fee for your first attempt on the 10-year exam if the exam fee has increased. The entire credit will be used to pay for the exam, and a zero balance will be left on your account.
If you've already pre-paid for 10 years, you will not need to pay until the 10 years pass. For example, if you pre-paid your program fee for 10 years in 2024, you will not have to pay an annual MOC fee before 1/1/2034.
The test center fee helps offset costs incurred for securing your seat at the Pearson VUE test center, as well as delivery of the exam itself.
The LKA is included in your annual MOC fee. If the LKA is not available in your discipline, you will not be required to pay the test center fee.
Yes. You will receive a 5% discount on any certificate you pay in advance. You can pre-pay up to nine years in advance by December 31 of the preceding year.
If you earned your initial certification before 1990, and you want to participate in an assessment for that certificate, you will need to pay the annual MOC fee. If you choose not to take an assessment, your fee will be forgiven at the end of the year. You will not lose certification based upon non-payment. You will not lose certification based upon non-payment.
Yes, those who are newly certified in internal medicine and those enrolled in an eligible fellowship program will receive an automatic MOC fee waiver.
ABIM recognizes fellowship training as an important part of lifelong learning and continuous professional development.
You can earn 20 MOC points for each year that you successfully complete accredited* fellowship training in an ABIM subspecialty. ABIM waives the annual MOC fees for any year during which you are in accredited fellowship training in an ABIM subspecialty.
Unaccredited training or training in a non-ABIM subspecialty does not qualify. Please contact your program director to verify whether your training is accredited.
*Accreditation Council for Graduate Medical Education (ACGME), or training completed in Canada that has been accredited by either the Royal College of Physicians and Surgeons of Canada or the Collège des médecins du Québec.
Longitudinal Knowledge Assessment (LKA®)
Eligibility and Enrollment
- All board certified physicians, except those in a grace year, can start participating in the LKA in their assessment due year.
- If you earned a certificate prior to 1990, you can use the LKA to help meet your assessment requirement to be reported as Participating in MOC.
- You can use the LKA to regain certification; however, because a decision on performance is not made until the end of the fifth year of participation, you will be reported as “Not Certified” until that time. Status will only change at that time if you pass the LKA and are meeting all other MOC requirements.
- If you are in a grace year, you are ineligible for the LKA and must pass the traditional, 10-year MOC exam by the end of your grace year to continue to be reported as “Certified.”
Learn more about what happens at the end of your five-year cycle.
You must open at least 500 out of the 600 questions offered over the course of your five-year LKA cycle to meet the LKA Participation Requirement.
The LKA Participation Requirement includes built-in flexibility to allow for life’s circumstances, such as weddings, vacations, funerals or anything that requires your time and energy. ABIM encourages you to take a break and not open questions when “life happens,” and come back when you’re ready.
At the end of each quarter:
- Questions you have opened will be scored.
- Questions you have not opened will count toward the maximum of 100 total questions you don’t have to open over five years.
Please note any unopened questions will not be scored and will expire at the end of the quarter, meaning you can't come back to them later.
The LKA performance standard is the score you must meet at the end of your five-year cycle to maintain your certification. It is also referred to as the "passing score." Although you will receive formative feedback on how you are doing along the way through quarterly progress reports, a summative determination is made at the end of the fifth year.
If your score meets or exceeds the passing score at the end of your five-year cycle, you can continue with the LKA.
If you failure to meet the performance standard, you will not lose certification, but you must pass the traditional, 10-year MOC exam the following year to remain certified.
Focused assessments cover the same topics as the general specialty blueprint with a greater proportion of questions in the area of focus, but at the same level of difficulty as this topic area outlined on the general blueprint.
Focused versions of the LKAs are created when the ABIM Specialty Board determines there is a need for a more specialized assessment for physicians who concentrate their practice on a specific area of medicine, such as medical oncologists who focus on breast cancer or gastroenterologists who focus on hepatology.
ABIM currently offers focused LKAs in two specialty areas with more targeted for launch in 2026:
- Internal Medicine: Inpatient
- Sleep Medicine: Obstructive Sleep Apnea Emphasis
Coming:
- Gastroenterology: Hepatology
- Hematology: Malignant
- Hematology: Classical (Nonmalignant)
- Medical Oncology: Breast Cancer
- Medical Oncology: Hematologic Neoplasms
You can review the new blueprints here when they become available in 2026.
The LKA requires a broadband connection. Both wired and wireless (802.11g and 802.11n) networks are supported.
Minimum system requirements (effective July 1, 2024, 12:00 a.m. ET):
- Windows: Windows 10+ with Microsoft Edge, Chrome or Firefox. The latest versions of Windows products can be downloaded from the Microsoft Download Center.
- Mac: Mac OS Mojave 10.14+ with Safari 13 or higher, Chrome or Firefox. The latest version of Mac products can be downloaded from the Mac Support site.
- Android: Android version 9.0 or higher.
- iOS: iOS version 13 or higher.
iPadOS: v15 (on iPad fifth generation or newer, iPad Air 2 or newer, iPad Pro).
The LKA uses the existing MOC exam blueprints to inform its content. In other words, the major medical content categories in any given specialty will be the same for all MOC assessments.
|
Quarter |
Opens |
Closes |
|---|---|---|
|
1 |
Jan. 1 |
Mar. 31 |
|
2 |
Apr. 1 |
June 30 |
|
3 |
July 1 |
Sep. 30 |
|
4 |
Oct. 1 |
Dec. 31 |
If you find that the LKA isn’t working for you, you can unenroll and register for a traditional, 10-year MOC exam (as long as the registration deadline hasn’t passed) through your ABIM Physician Portal.
No, you will not be able to enroll in the LKA while your exam results are pending. If you are unsuccessful once the exam results have been released, and you wish to switch to the LKA, you can do so as long as it is before the June 30 LKA enrollment deadline.
Please note: exam results can take up to three months to be released. This means that exam results could be pending beyond the LKA enrollment deadline of June 30. If this happens, you would still have the opportunity to take the traditional, 10-year MOC exam or the ACC/ABIM Collaborative Maintenance Pathway (CMP) in cardiovascular disease and its subspecialties.
The LKA is designed to help you measure your medical knowledge over time. This means you’ll have the opportunity to change your approach and improve your performance during your five-year cycle if you find you're not performing at the level you expected.
While the LKA is intended to be both a learning tool and an assessment focused on medical knowledge that a physician typically wouldn’t need to research extensively in day-to-day practice, you should still take it seriously and treat it like an assessment.
Some physicians may find that their typical approach to keeping current with medical knowledge is effective and no additional studying is required. Others may want to use the feedback provided as part of the LKA to address knowledge gaps to ensure that their knowledge remains broad and current. This feedback includes the correct answer to the question, the rationale for the right and wrong answers, and references.
In addition, your quarterly progress reports (offered in your second year of LKA participation and every quarter afterwards) will give you helpful information to adjust your approach and focus your studies as needed.
The number of questions offered through the LKA is the same for all specialties. ABIM is exploring models that may reduce the number of questions for disciplines that have overlapping content in the future.
LKA Progress Reports and Assessment Feedback
Access to a quarterly progress reports will be available after you have answered enough questions. For most physicians, that will happen early in their second year of taking the LKA. The quarterly progress reports will let you know how you are performing relative to the current passing standard, helping you understand areas you are performing well in as well as those in which you may want to focus for future study.
The intention of the LKA quarterly progress report is to offer you continuous feedback about your performance on the LKA as you progress through a five-year cycle. There are four sections on the LKA quarterly progress report:
- Your timeline:
- Shows you what quarter the current progress report covers.
- Your performance:
- Displays your current score as of the latest quarter covered in the report along with previous scores.
- The current passing score is also displayed for comparison with your current score.
- Group performance:
- Displays a distribution of scores for all participants who received a score for that quarter.
- Shows you where your current score, the passing score and the average score fall in the distribution.
- Recent content area performance:
- Shows you how many items you got correct and incorrect within each content area over the past year.
- Shows you how many items you were confident or not confident about for items you got correct and incorrect within each content area over the past year.
For additional information, please watch the LKA quarterly progress report video.
Quarterly progress reports covering a given quarter are released three to four months after that quarter has ended. To ensure the accuracy and integrity of the scores, ABIM conducts a rigorous multi-step scoring and quality assurance process. This quality assurance process includes, but is not limited to, item analysis, key validation, item calibration, equating and scoring.
Specialty Knowledge Gaps
Categories that are represented by very small numbers (sparse data) may result in larger standard errors which are often less reliable than data represented by large numbers.
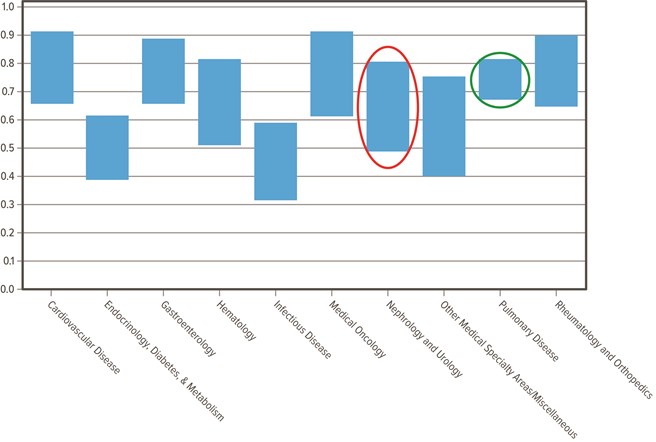
This example graph shows:
- Nephrology and Urology (red circle) is an example of a larger standard error (less reliable)
- Pulmonary Disease (green circle) is an example of a smaller standard error (more reliable)
Equating is a statistical process used to convert scores from different examinations to a common score scale for purposes of comparability and equivalence. ABIM does not compute equated scores for medical content area scores—only for overall scores.
For reporting purposes, smaller top-level blueprint areas are combined with other similar blueprint areas in order to provide more meaningful and stable information.
U.S. Census Bureau classifications for region have been used to identify physicians in the Northeast, Midwest, South and West. You can view which states are included in each region on the U.S. Census Bureau's website.
Each question on the examination falls into a specific blueprint area and tests a specific cognitive task. Definitions for the tasks can be found in the content outline for the MOC exam. Please note that not every discipline incorporates tasks in its respective MOC blueprint.
A blueprint is a table of specifications that determines the content of each assessment. It is developed by the Approval Committee for each discipline and reviewed annually. The discipline's Specialty Board or Advisory Committee must also approve the exam blueprint. The blueprint is based on analyses of current practices and understanding of the relative importance of the clinical problems in the specialty area. The blueprint also includes the target percentage of questions from each primary medical content category on the assessment. This ensures appropriate and equal representation of the content categories between assessment administrations. Changes to the composition in the blueprint usually follow trends in current practice. Read more about ABIM's assessment process.
The Specialty Knowledge Gaps Reports are based on up to three years of performance data. Each physician can respond to up to 80 live items per year. Over time more items will be included in the reports and can provide more accurate and reliable information.
You can learn more about the LKA by visiting our dedicated LKA website.
Proposed Pilot Model Pathway
Pilot Eligibility
The pilot program isn’t currently active. There are several levels of approval needed by ABIM and the American Board of Medical Specialties before the pilot program can be implemented. ABIM will be communicating with eligible applicants and the graduate medical education community where possible to make sure potential candidates are aware of the opportunity should it become available.
Pilot participants are physicians who trained in internal medicine residency internationally (or trained in an ACGME-I accredited residency) and have successfully completed an accredited fellowship in the U.S. or Canada, and who meet the qualifications to be considered an “exceptionally qualified candidate” per ACGME criteria. Pilot participants may apply for the ABIM Internal Medicine Certification Examination only once fellowship is successfully completed and competency in all domains is documented by the accredited training program in FasTrack.
ABIM will be using the longstanding ACGME definition of “exceptionally qualified” (see ACGME Common Program Requirements (Fellowship), III.A.1.c). ABIM’s pilot may be able to shed light on whether there is a shared perspective on what characterizes an exceptionally qualified candidate.
Additionally, the ACGME criteria to be considered “exceptionally qualified” call for a competency-based performance evaluation at 12 weeks of fellowship training.
Yes, candidates who have successfully completed ACGME-accredited fellowship within the prior seven years will be considered Board Eligible, consistent with ABIM’s Board Eligibility policy.
This pilot program will be available in all ABIM subspecialty disciplines where accredited training is required, regardless of training length. Pilot participants will be subject to all other initial certification eligibility requirements, e.g., licensure requirements and ABIM Board Certification in Internal Medicine prior to application to the ABIM Subspecialty Certification Examination.
Yes.
The ABIM pilot does not affect match rules. Eligibility for the match is determined by the National Residency Matching Program (NRMP). Many pilot participants may have entered ACGME-accredited fellowships through the NRMP.
Pilot Requirements
Not specifically. Program directors would evaluate the fellow’s competence and their Board Eligibility in the discipline they are training in. The six general core competencies for internal medicine and subspecialties are the same at the competency level and similar at the milestone level. If competency isn’t achieved in residency training, it should become apparent in fellowship. ACGME criteria to be considered “exceptionally qualified” also call for a competency-based performance evaluation at 12 weeks of fellowship training. The Internal Medicine Certification Examination serves as an assessment of medical knowledge and judgement in internal medicine.
No. There is a requirement that Board Eligibility is tied to competency demonstrated by the successful completion of accredited training in the U.S. or Canada. Pilot participants will not be eligible to apply for the Internal Medicine Certification Exam until they document competency through successful completion of their accredited fellowship training program.
No. Physicians must be certified in internal medicine at the time they apply for subspecialty certification. Since the Internal Medicine Certification Exam is administered in the summer, it would not be possible to meet this requirement for fall Subspecialty Certification Exams.
Pilot Outcomes
Yes, if they pass the Internal Medicine and Subspecialty Certification Exams. Pilot participants will be held to the same fellowship training standards as other fellows, they will take the same certification examinations as other initial certification candidates (both in internal medicine and their subspecialty) and, if successful, will earn the same certificates as other diplomates (both in internal medicine and their subspecialty). They will be held to the same requirements and standards as other diplomates in the Maintenance of Certification (MOC) program.
There are many potential inquiries that this pilot will address. Some of the primary questions ABIM will seek to answer include, but are not limited to:
- Do these physicians pursue Board Certification?
- How do they perform on ABIM assessments?
- What is their practice setting post-training?
- Do they remain in the U.S.?
Does the pilot affect in any way the number of U.S. medical graduates matching into accredited fellowship programs?
ABIM is hopeful that through information gathered from the pilot, ABIM can decide whether the pilot is viable (Is it possible for physicians to do it?), feasible (Is it easily integrated into the training process? What are the outcomes for pilot participants?) and scalable (Can it be applied across fellowships in different states and different disciplines? Does it show evidence of a standardized concept for an “exceptionally qualified candidate”?).
After extensive data collection and careful analyses, the ABIM Council will decide whether or not to apply to the American Board of Medical Specialties to make the pilot program an official, standard pathway to ABIM Board Eligibility.

